One year after the Africa Centres for Disease Control and Prevention (Africa CDC) declared mpox a continental emergency, countries have strengthened their responses and are reporting progress in controlling the disease.
Coordinated action among governments, the Africa CDC, the World Health Organization (WHO), communities and partners has helped improve disease surveillance, expand laboratory testing, mobilize vaccination drives and improve treatment for people with mpox.
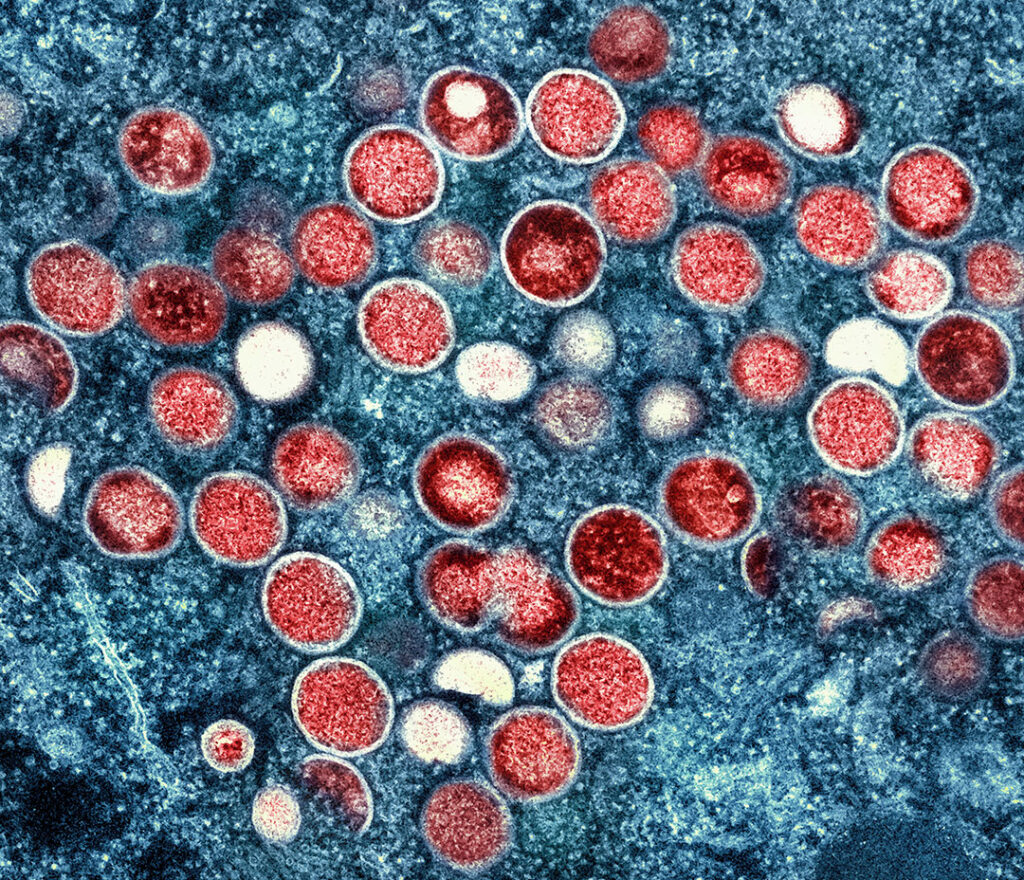
The disease is similar to smallpox and is caused by a virus. It causes flu-like symptoms such as fever and chills, and a rash that can take weeks to clear.
“We have seen a clear downward trend in mpox cases across the most affected countries thanks to the commitment of our member states and the support of our partners,” Director-General Dr. Jean Kaseya said in the Africa CDC’s biweekly media briefing on August 15.
“In the past six weeks, confirmed mpox cases have dropped by 34.5% compared to the previous six weeks. The Democratic Republic of Congo (DRC), Sierra Leone, Uganda and Burundi account for over 80% of 2025’s cases but have seen significant declines.”
Mpox has affected 28 African countries since August 14, 2024, when the WHO declared it a public health emergency of international concern. More than 174,000 suspected cases have been reported on the continent, but that includes just under 50,000 confirmed cases and about 240 deaths — both figures that experts say are likely undercounts because of weak diagnostic capacity.
In the last year, however, mpox diagnostics in Africa have expanded significantly, from two laboratories in the DRC in January 2024 to 69 in August 2025, and from one to 56 in Burundi. Twenty-one countries have generated more than 4,000 mpox genomic sequences, and more than 1,000 community health workers have deployed, with an additional 10,000 trained to support detection, vaccination and treatment.
Dr. Otim Patrick Ramadan, program area manager emergency response at WHO Regional Office for Africa, lauded the synergy between his organization and Africa CDC.
“Our collective efforts have been crucial in strengthening measures for an effective response,” he said in an August 14 statement. “It is critical to sustain what works, which includes rapid case detection, timely targeted vaccination, strong laboratory systems, and active community engagement.”
The Africa CDC and WHO recently updated their continental mpox preparedness and response plan and co-led its implementation through a continental Incident Management Support Team. The plan serves as a map to finish the response phase and transition to routine prevention, response and treatment programs.
“With limited resources, there is a critical need to be more efficient which means working as one team, with one plan budget and monitoring framework,” Africa CDC Deputy Continental Incident Manager Yap Boum said in a statement.
The Africa CDC and WHO have worked jointly with affected countries to boost response capacity. They have procured, shipped and distributed more than 6 million doses of mpox vaccine, with 951,000 doses administered and nearly 900,000 people receiving at least one shot. Of the 22 countries with active transmission, 13 have vaccine deployment plans and eight have begun vaccinating high-risk groups and their contacts.
Some countries, such as Côte d’Ivoire, have brought outbreaks under control, reporting 42 days with no new cases. Angola, Gabon, Mauritius and Zimbabwe have exceeded 90 days with no confirmed infections.
Despite the progress, challenges remain. These include limited access to vaccines, competing emergencies, funding gaps, inadequate access to care, and stigma that prevents people from seeking care. Widespread violent conflict in eastern DRC also is disrupting response efforts.
“Our priorities for the next six months are to expand community-based surveillance in high-risk areas, continue to procure and distribute essential supplies to hotspots, support the integration of mpox response into other health programs for sustainability, support targeted vaccination and advocate for more funding for vaccine deployment,” Otim said.