ADF STAFF
Deep inside every human cell, tiny structures known as mitochondria serve as the powerhouse, providing the energy needed for the lungs to breathe, the heart to beat and muscles to contract.
New research indicates that COVID-19 damages the body — particularly the lungs — by attacking those powerhouses. The ensuing damage can be enough to trigger the affected cells to destroy themselves, creating a potentially fatal cascade of damage.
Researchers believe the attack on mitochondria is a key part of why COVID-19 can be so deadly for people with existing health issues, such as high blood pressure or diabetes, which already damage the tiny structures. They also suggest that damaged mitochondria may be behind some of the symptoms of the condition known as long COVID.
“Viral proteins fragment the mitochondria, depriving cells of energy and interfering with their oxygen-sensing capability,” Dr. Stephen Archer wrote in The Conversation.
Archer leads the Department of Medicine at Queen’s University in Ontario, Canada and is conducting research to find a way to protect mitochondria from being destroyed by viral attacks.
Those attacks start soon after a person is infected with COVID-19, according to Archer.
The battle between mitochondria and the COVID-19 virus is one that goes back to the beginning of life on earth. Back then, mitochondria’s ancestors lived as free-floating bacteria at risk of attack from viruses known as bacteriophages, or bacteria eaters.
Eventually, those ancestral mitochondria found protection by moving inside cells. The arrangement provided the cell with a boost of energy and shielded the mitochondria from attacks. The mutually beneficial arrangement continues to this day.
During a COVID-19 infection, the SARS-CoV-2 virus invades cells in the airways. Once inside, it turns the machinery of the cell into a virus factory, churning out new virus copies that spread with every unmasked cough, sneeze or breath in a confined space.
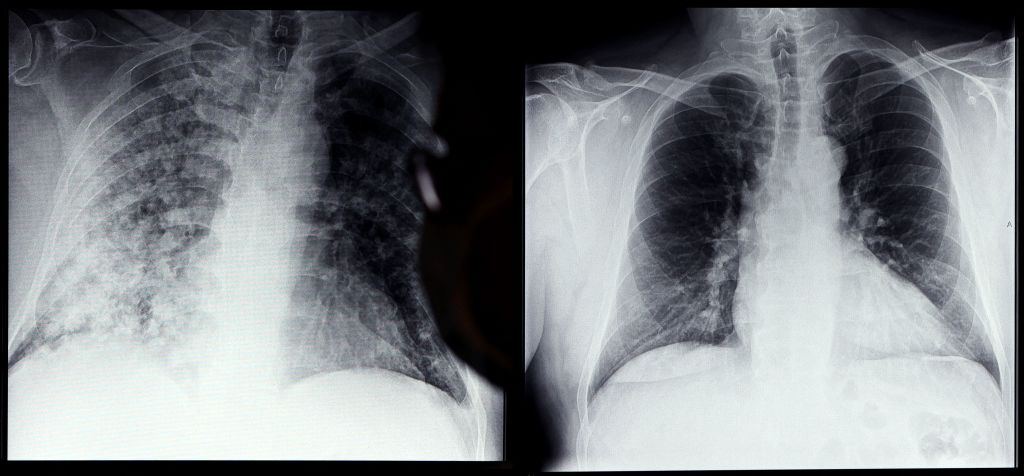
In the lungs, COVID-19 attacks the cells lining the pulmonary artery, which carries oxygen-rich blood to the heart to be distributed across the body.
In addition to powering the cells that make up the artery, oxygen-sensitive mitochondria also regulate the flow of blood in the lungs. In essence, when cell mitochondria detect lower-than-normal amounts of oxygen in a portion of the lungs — due to COVID-19 related pneumonia, for example — they trigger the blood vessels in that section to constrict. That way they ensure that the blood moving through the lungs stays in areas where oxygen levels are highest.
“By damaging the mitochondria in the smooth muscle cells of the pulmonary artery, the virus allows blood flow to continue into areas of pneumonia, which also lowers oxygen levels,” Archer wrote.
Health conditions such as high blood pressure and diabetes create a chemical imbalance in the body that weakens cell mitochondria, making them more vulnerable to attack by COVID-19, according to Dr. Ralph Ryback and his co-researcher, Dr. Alfonso Eirin of the Mayo Clinic in Minnesota.
By crippling mitochondria, COVID-19 undermines the body’s systems at their most basic level. The breakdown of the cellular powerhouse, and the chain-reaction of cell destruction that follows, may explain the lingering effects of COVID-19 known as long COVID, according to infectious disease expert Gerald Evans, who was part of Archer’s research team in Canada.
“The predominant features of that condition — fatigue and neurologic dysfunction — could be due to the lingering effects of mitochondrial damage caused by SARS-CoV-2 infection,” Evans wrote.